Medical
For the 2026 plan year, you will choose between the PPO Low Plan and the PPO High Plan, using the Cigna PPO network. We have a new free Garner benefit that helps you find the highest quality doctors while saving you up to $5,000 individual / $10,000 family in healthcare costs. This benefit is included for both medical plan options. There are no changes in team member premiums for 2026. There are also updates to the prescription drug benefits for 2026 with VeracityRx as the new pharmacy benefits provider.
In-network preventive care services, such as annual check-ups, are covered in full for both plans. As a reminder, these services need to be coded as preventive to be paid in full by the plan.
The medical plans are administered by Nova Healthcare. Nova Healthcare processes your claims and eligibility updates. HealthJoy, your healthcare guidance app, helps improve your healthcare experience while saving you time and money. We encourage all medical plan members to use the HealthJoy app when you need medical services.
Although the plans include out-of-network coverage, your costs are significantly lower if you remain in the Cigna PPO network. You may access Cigna PPO network information by using the HealthJoy mobile app or on Nova’s website.
In-Network Medical Summary
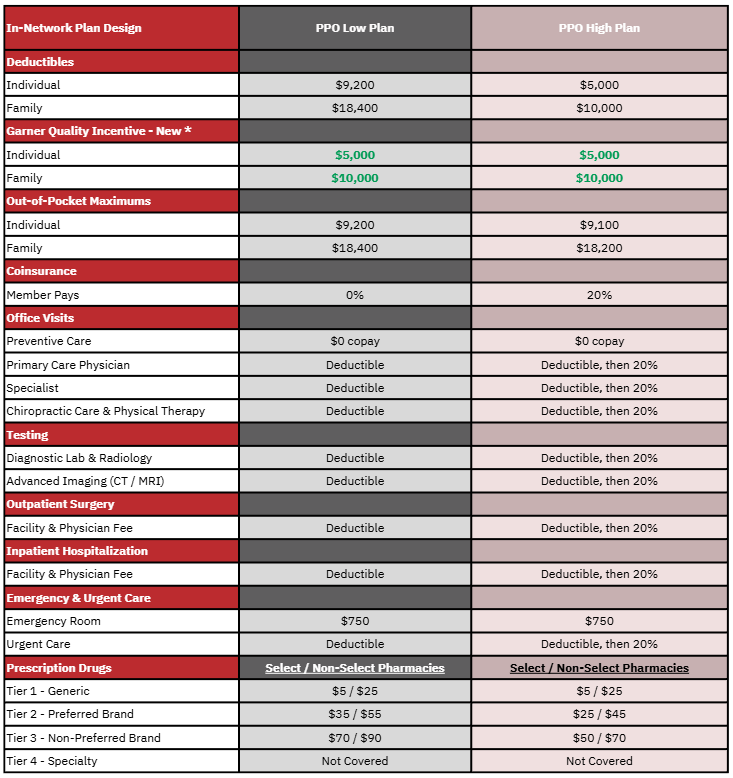
*Emergency room and prescription drug benefits are not eligible for the Garner high-quality incentive.
Other Benefit Summary Notes
- Higher out-of-pocket costs for out-of-network services.
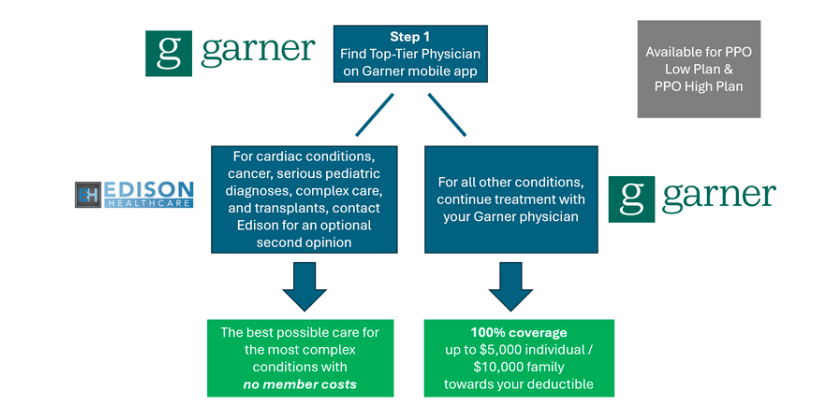
Garner: Quality-Incentive Benefit
Garner Health is a free benefit that helps you find the highest quality doctors while saving you money. For both plan options, when you use the Garner app, find a recommended doctor, and visit that doctor, you will receive 100% coverage! Emergency room visits and prescription drugs are not eligible for the Garner incentive benefit.
The best doctors are often the least expensive. Missed diagnoses, unnecessary surgeries, and bad health outcomes are costly. By setting you up with the best doctors, you not only get better care, but the cost is lower for both you and Jim Ellis. As a result, Jim Ellis covers your medical bills when you use Garner.
Team members receive up to $5,000 individual and $10,000 dependent(s) when you visit a top-tier provider. Garner can be used for all kinds of care:
- Primary Care Physicians and Specialists
- Simple labwork and diagnostics
- As long as a top-tier physician orders the test, it will be covered, regardless of which lab is used.
- For invasive labwork and complex imaging, like MRI or CT, these services will be covered if they are provided by a Garner approved provider.
- Search by type of provider, procedure, or condition
- Click "Find Care" in the app and type what you are looking for.
- Examples: colonoscopy, MRI, lower back pain, hand surgery, pinched nerve, sleep apnea, etc.
- Physicians Assistants (PAs) and Nurse Practitioners
- If you have an appointment with an approved doctor and a nurse practitioner in their practice sees you instead, the costs from that visit will be eligible for the incentive. Even if it is after your service date, message the Concierge through the Garner Health app and ask to have the PA or nurse practitioner added to your Care Team.
- Nurse Practitioners and Physicians Assistants are not listed in the Garner app. Contact the Garner Concierge to confirm whether your Nurse Practitioner is approved for the benefit. If they practice under a Garner approved, provider, the Concierge can add them to your Care Team.
How It Works
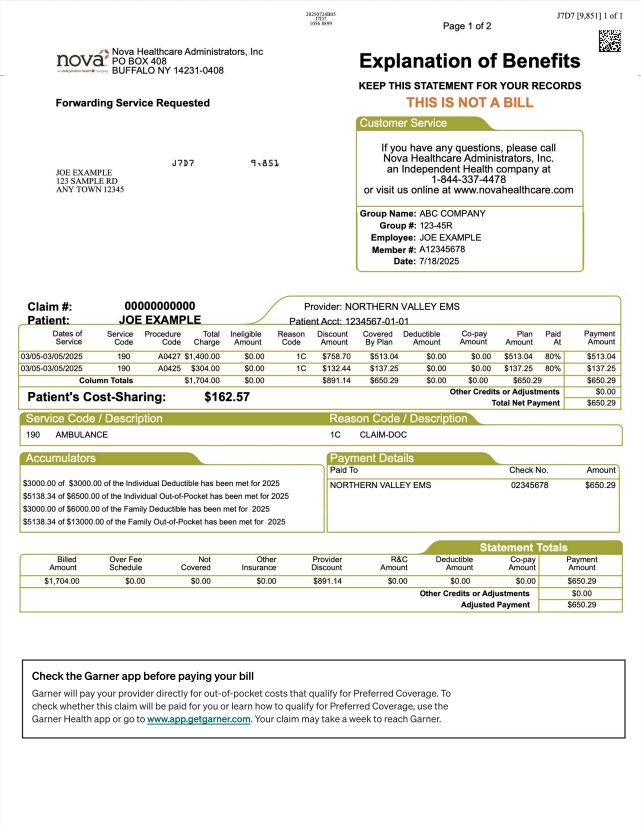
- A member must use Garner to get a recommendation before visiting the provider.
- Visit the provider recommended by Garner and provide your Medical ID Card at the time of service.
- Since most services are subject to the deductible, your doctor should not bill you at the time of service.
- Following your medical service, the claim will be processed by Nova, and the Garner incentive benefit will be applied before calculating your patient responsibility.
- If you have a patient responsibility, this will be indicated on your Explanation of Benefit (EOB).
- As a reminder, do not pay your physician until you receive the Explanation of Benefits (EOB) from Nova. In some cases, provider invoices are generated before the claims are processed. It is important to wait until the claim has processed to confirm your patient responsibility before paying your bill.
- If a Garner recommended provider bills you at the time of service, please contact the Garner Health Concierge for assistance.
Get Started with Garner
- Visit getgarner.com/signup
- Download the Garner Health app
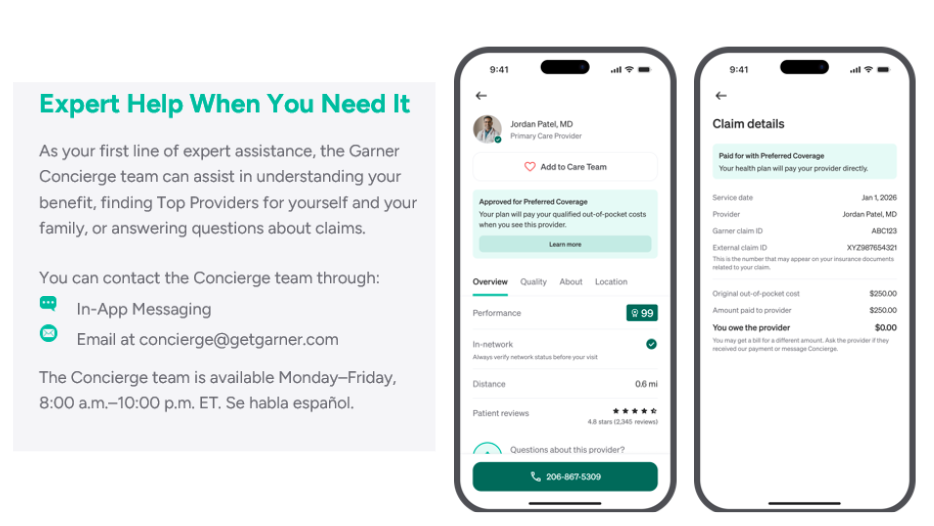
- Email concierge@getgarner.com, or call 866-761-5147 to locate the top doctors in your area
- Check out the Garner Guide - for general information about the new Garner benefit and to help you with your questions: https://garnerguide.com/jim-ellis.
You can view more information on Garner on this webinar.

Centers of Excellence Second-Opinion Program
Garner Health is your first stop to find high-quality providers. The Edison Centers of Excellence program is a voluntary, second-opinion, high-quality resource for specific diagnoses. The Edison Smart Care Centers are available with no member cost for these conditions.
Distance and cost should never get in the way of you receiving the best possible medical care. Our team members who are enrolled in medical will have full access to Edison’s Smart Care Network. All possible barriers have been removed for the best care and all travel expenses will be covered for you and a companion. All team members, spouses, and dependent children who are enrolled in the
medical plan are eligible. This is ZERO COST HEALTHCARE at AMERICA’S BEST MEDICAL CENTERS for the diagnosis types listed below.
- Cancer
- Cardiac
- Transplant
- Pediatric
- Complex Care
Tools & Resources for High-Quality Healthcare
Nova Healthcare
Although the plans includes out-of-network coverage, your costs are significantly reduced if you remain in the Cigna PPO network. You may access Cigna PPO network information as follows:
- www.novahealthcare.com/member
- Find a Provider
- Click on the Cigna Provider directory, select PPO for the plan, and follow search instructions.
OR
Access https://hcpdirectory.cigna.com/web/public/consumer/directory/search or call 833-891-9368
Nova Explanation of Benefits (EOB)
Access your Nova Explanation of Benefits (EOB) for claim details and deductible and out-of-pocket accumulator information.
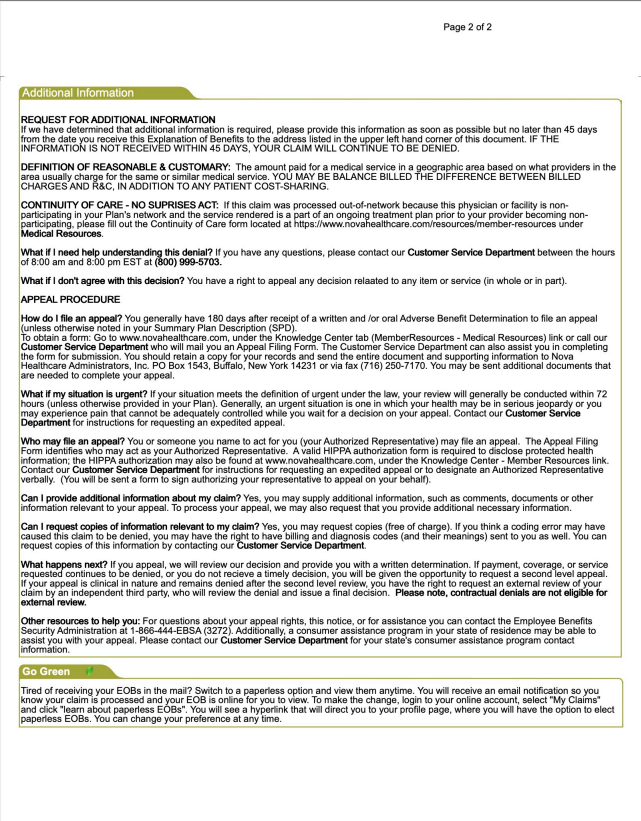
Sample ID Card
You will provide your Nova Healthcare ID Card to your Cigna PPO doctor or hospital when you schedule medical care, and pay your copay at the time of service.
New ID Cards will be provided for all medical plan participants for 2026.
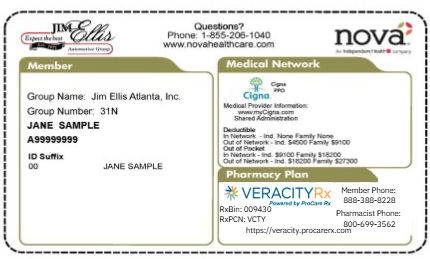
Prescription Drug Coverage
There are some updates to the prescription drug benefit for 2026. VeracityRx is your new pharmacy benefit provider, and VeracityRx will handle your prescription drug claims and customer service. As a reminder, the prescription drug benefit is included in the medical plan out-of-pocket.
The 2026 pharmacy benefit uses a Select / Non-Select pharmacy network. Most pharmacies can fill your prescriptions, but if you use a Non-Select pharmacy, your copay will be higher. Select pharmacies include most pharmacies, while Non-Select pharmacies include CVS, Walgreens, Target, and Rite-Aid.
Retail and 90-Day Supply Benefits
Although the 2026 prescription drug plan does not include a mail order benefit, you can elect to get a 90-day fill at Select pharmacies for 2x the 30-day supply copay. Please note that a 90-day fill is not available at Non-Select pharmacies.
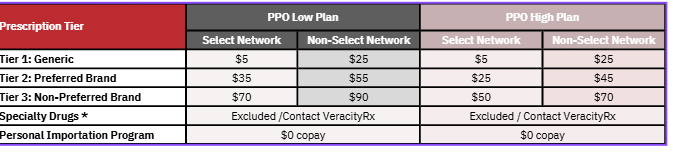
Veracity Rx Mobile App
Personal Importation Program
Certain medications can be obtained internationally from Canada. When medications are obtained this way, the cost to the member is $0 copay. If the member chooses not to participate in the PIP and to fill at a retail pharmacy, the cost to the plan participant is 50% of the cost of the medication and will not apply to the medical plan maximum out-of-pocket.
How to Enroll
- Access veracity-rx.com and complete the Enrollment Form. If you are unable to enroll online, call 888-388-8228.
- Be on the lookout for an email from VeracityRx with next steps.
- Contact your healthcare provider to have a new prescription sent to the pharmacy partner. Instructions will be provided in email on step #2 above.
Specialty Drugs
Although specialty drugs continue to be excluded on your health plan, VeracityRx may be able to help you find the best price for your specialty medications. Contact VeracityRx Pharmacy Services at www.veracity-rx.com for more information.
